Microdosing vs Antidepressants: Comparing Psilocybin and SSRIs for Mood Support
Selective serotonin reuptake inhibitors (SSRIs) have long been a first-line treatment for depression and anxiety disorders. These pharmaceutical antidepressants are widely used and have helped many people manage their mood disorders. In recent years, however, there’s been growing interest in natural antidepressant options and mental health alternatives. One of the most talked-about is microdosing psilocybin, or taking tiny doses of “magic mushrooms,” as a potential mood booster for depression. This microdosing vs antidepressants debate raises important questions: Can a small dose of shrooms serve as a psilocybin depression alternative, or even complement traditional medication? How do shrooms and SSRIs compare in terms of effectiveness, side effects, and safety?
In this post, we’ll provide a trustworthy, evidence-based comparison between psilocybin microdosing and SSRIs. We’ll summarize current research on psilocybin for depression, explain how microdosing works differently from SSRIs, and outline key differences in onset time, dependency risk, side effects, long-term effects, regulatory status, and accessibility. Importantly, we’ll highlight safety considerations – especially if someone is considering combining medication and mushrooms – and emphasize the need for medical guidance. Finally, we’ll introduce some approachable microdosing products and a program from Sugar Magnolia that can support those curious about this natural mood booster. Always remember: any changes to your mental health treatment should be made in consultation with a qualified healthcare provider.
What Are SSRIs (Antidepressants)?
Selective Serotonin Reuptake Inhibitors (SSRIs) are a class of prescription antidepressant medications commonly used to treat major depression, anxiety disorders, and related conditions. SSRIs work by increasing serotonin levels in the brain – they block the reabsorption (reuptake) of the neurotransmitter serotonin, making more serotonin available to improve communication between brain cells. Since serotonin is associated with mood regulation, boosting its activity can help relieve depressive symptoms over time.
SSRIs (such as Prozac, Zoloft, Lexapro, and others) are popular because they generally have fewer severe side effects than older antidepressants. They are typically taken once daily, and one drawback is that they take time to exert their full effect. It may take anywhere from 4 to 8 weeks to feel the full therapeutic benefits of an SSRI. Patients are usually advised to keep taking the medication consistently during this period, even if they don’t notice immediate improvement.
Despite their effectiveness for many individuals, SSRIs are not a perfect solution. Common side effects of SSRIs include weight gain, sexual dysfunction, insomnia, gastrointestinal issues, and drowsiness, among others. While these side effects are often manageable, they can be persistent and impact quality of life in some cases. Another consideration is that SSRIs are typically used long-term; some people remain on them for years to maintain mood stability. When it comes time to stop, SSRIs must be tapered gradually under medical supervision – stopping suddenly can lead to antidepressant discontinuation syndrome, which involves withdrawal-like symptoms. (Notably, SSRIs aren’t considered addictive in the way drugs of abuse are, but patients can become physically dependent on them to feel “normal,” hence the need for a careful taper.)
It’s also worth noting that, for a significant minority of patients, SSRIs may provide only partial relief or none at all. Antidepressant drugs have modest efficacy on average, can cause unpleasant side effects, and often patients experience relapse of depression after stopping the medication. This is why researchers and patients alike have been exploring new approaches – including psychedelic therapies – to treat depression. Enter psilocybin, the active compound in “magic mushrooms,” which has garnered attention as a novel way to address mood disorders.
What Is Psilocybin Microdosing?
Psilocybin microdosing refers to taking very small, sub-hallucinogenic doses of psilocybin – usually about 1/10 to 1/20 of a typical psychedelic dose – on a regular schedule. For example, someone might take a tiny dose of dried psilocybin mushrooms (or an equivalent capsule/gummy) every third day. The goal is not to experience a full psychedelic trip, but rather to subtly boost one’s mood, creativity, focus, or overall well-being while remaining fully functional in daily life. In other words, microdosing aims to harness psilocybin’s potential as a natural mood booster without the intense “journey” that a large dose would induce.
Psilocybin is a naturally occurring compound found in certain mushroom species (colloquially called “magic mushrooms” or simply “shrooms”). When ingested at higher doses, it binds strongly to serotonin 5-HT2A receptors in the brain, leading to profound changes in perception, cognition, and mood. In microdose amounts, the effect is much milder – often sub-perceptual – but still pharmacologically active. Many people who microdose report that it elevates their mood and energy, reduces symptoms of depression and anxiety, and enhances creativity and focus, all without causing hallucinations. In fact, survey studies have found that thousands of microdosers self-report positive mental health benefits, including sustained improvements in negative mood (especially depression), along with increases in positive mood, energy, and healthier habits. These anecdotal outcomes have led some to hail microdosing as a “natural antidepressant” approach.
However, it’s important to stress that scientific evidence on microdosing is still limited. Unlike SSRIs, which have been tested in large clinical trials, psilocybin microdosing remains an experimental practice. Early research is mixed: open-label and survey studies suggest microdosing may indeed correlate with lower depression, anxiety, and stress levels, but more rigorous placebo-controlled trials show more lukewarm results. For example, one notable placebo-controlled study found no significant difference in psychological outcomes between people microdosing (without knowing it) and those taking placebos, indicating that expectations may play a large role in perceived benefits. Scientists are split on whether the benefits some microdosers experience are primarily a placebo effect or due to real pharmacological changes. More research is underway to resolve these questions, as major institutions ramp up studies on low-dose psychedelics.
Mechanistically, psilocybin in any dose works differently from an SSRI. Psilocybin is a serotonin receptor agonist – it mimics serotonin at certain receptors (notably 5-HT2A) and can induce downstream effects like increased neuroplasticity and altered brain network connectivity. In fact, lab studies show that psychedelics activate receptors that help brain cells form new connections, which may underlie their rapid antidepressant effects observed at higher doses. By contrast, SSRIs indirectly modulate serotonin by preventing its reuptake, and do not cause a sudden change in network connectivity; their mood effects develop gradually. This difference in pharmacology means microdosing “shrooms” might offer a more direct (albeit subtle) brain reset or cognitive flexibility boost, whereas SSRIs provide steady mood stabilization over time. Of course, microdosing’s effects are gentle – users are not experiencing breakthroughs or hallucinations – but even sub-perceptual doses could be tuning the brain in ways distinct from conventional antidepressants.
Legally, it must be noted that psilocybin remains a Schedule I controlled substance under U.S. federal law (and is similarly prohibited in many other countries). Outside of clinical trials and a few special jurisdictions, psilocybin use is illegal. Nonetheless, decriminalization efforts and research exemptions are gradually expanding. For instance, in 2023 the U.S. FDA released draft guidance to help researchers design psychedelic drug trials, signaling official interest in psilocybin’s therapeutic potential. As public interest grows and some cities or states enact reforms, psilocybin microdosing has moved somewhat into the mainstream discussion – but it’s still largely an underground or gray-area practice for now. Anyone considering it should be aware of local laws and the fact that product quality can vary greatly if obtained from unregulated sources.
Psilocybin vs. SSRIs: How Do They Work Differently?
It’s clear that psilocybin microdosing and SSRIs take very different approaches to influencing mood and brain function. A quick recap of their mechanisms highlights the contrast:
- SSRIs increase serotonin by reuptake inhibition: By blocking the reuptake pumps on neurons, SSRIs cause serotonin to accumulate in the synapses. This gradually amplifies serotonin signaling over weeks. The effect is like raising the “baseline” serotonin tone of the brain. Mood improvement tends to be steady and subtle once it kicks in, and patients must continue daily dosing to maintain the effect.
- Psilocybin (even in microdoses) directly stimulates serotonin receptors: Psilocybin is converted in the body to psilocin, which binds to various serotonin receptors. The most important is the 5-HT2A receptor, which triggers a cascade of changes in brain activity. Even a microdose will transiently engage these receptors more than usual, potentially enhancing neuroplasticity (the brain’s ability to form new connections) and “resetting” certain neural circuits associated with mood and cognition. Notably, psilocybin and SSRI medications rebalance brain dynamics in depression via distinct pathways – SSRIs gently adjust neurotransmitter levels, while psilocybin more directly alters the communication patterns between brain regions (especially those related to rumination, fear, and cognitive flexibility).
- Emotional and subjective effects: Many SSRI users describe a blunting of extreme emotions – they feel less depressed or anxious, but sometimes also less intense joy or passion (a phenomenon sometimes called “emotional flattening”). Microdosers, on the other hand, often report a subtle enhancement of emotional well-being – not euphoria per se, but a feeling of being more “in tune” or optimistic, with preserved (or even heightened) sensitivity to positive feelings. Of course, these subjective reports vary from person to person.
- Onset of action: Perhaps one of the biggest practical differences is speed. SSRIs require patience; as mentioned, it can take a month or two before an SSRI yields noticeable mood improvement. In contrast, psilocybin’s effects (even at low dose) occur the same day as ingestion. Individuals who microdose often can tell on the day of a microdose that their mindset is a bit lighter or more upbeat. In clinical settings with high-dose psilocybin, patients have sometimes experienced relief within hours or days of a single psychedelic session. One comparison often cited is that antidepressants can take 4–8 weeks to kick in, whereas psychedelics (at a macrodose) induce rapid relief within hours. Even though microdosing doesn’t cause dramatic acute effects, many users feel some positive effects within the first week, which is far quicker than waiting two months on an SSRI. Moreover, early research suggests that just one or two full psilocybin sessions can produce antidepressant effects lasting at least six months to a year in some patients – a durability that standard antidepressants generally do not match without continuous use.
In summary, SSRIs are a slow-buildup, daily maintenance approach to regulating mood via serotonin availability. Psilocybin (microdosed) is a fast-acting, intermittent approach that directly tweaks serotonin receptors and potentially promotes neural flexibility. Both aim to alleviate depression and anxiety, but they “attack” the problem from different angles. This complementary difference has led some experts to wonder if microdosing could be used alongside or in sequence with SSRIs – but as we’ll discuss later, combining them must be done very cautiously (if at all).
Before diving into safety, let’s lay out a side-by-side comparison of microdosing vs. antidepressants across several key dimensions:
Microdosing vs Antidepressants: Key Differences
To better understand how psilocybin microdosing stacks up against SSRIs, here’s a comparison of several important factors:
| Factor | Psilocybin Microdosing | SSRIs (Antidepressants) |
| Onset of Benefits | Often rapid – users may sense subtle mood lift on dosing days, and anecdotal reports show improved well-being within days to a couple of weeks. (Psychedelic effects manifest within an hour of dosing, though microdoses are very mild) | Delayed – typically takes 4–8 weeks for full antidepressant effect to be felt No immediate mood boost; patience is required while the medication builds up in the system. |
| Dependency Risk | Low physical dependence – Psilocybin does not cause physiological addiction. There’s no known withdrawal syndrome from stopping microdosing. (Tolerance can develop if used too frequently, which is why protocols include off-days.) Psychologically, habit-forming potential is considered low. | Low addictive potential, but possible dependence – SSRIs are not habit-forming in the way opioids or nicotine are, and cravings are not an issue. However, the body adapts to them, so stopping abruptly can cause discontinuation (withdrawal) symptoms like dizziness, irritability, and flu-like feelings Tapering off is needed after long-term use. |
| Side Effects | Mild and transient for most – At micro doses, side effects (if any) might include slight insomnia on dose days, mild anxiety or headache, or subtle physiological changes. Generally, people tolerate microdosing well and can go about daily activities. Notably, classic psychedelic side effects like perceptual changes are not present at micro levels. (Serious risks like psychosis are extremely rare and typically associated with high doses in predisposed individuals.) | Common and sometimes persistent – Side effects of SSRIs can include weight gain, sexual dysfunction, nausea, diarrhea, insomnia or drowsiness, dry mouth, and increased nervousness. Many of these occur as the body adjusts and may linger throughout treatment. Some individuals also report emotional blunting. Side effect profiles vary by person and specific SSRI. |
| Long-Term Effects | Unknown/Under-studied – There is limited research on the long-term effects of regular microdosing. So far, no severe long-term harms have surfaced in studies, but science is still catching up. There is concern about potential heart valve issues with chronic use of any 5-HT2B agonist (a receptor psychedelics also hit), but this remains theoretical at micro doses. Many microdosers take periodic breaks to avoid building tolerance. Overall, the safety and long-term effects of microdosing remain under review. | Established but requires ongoing use – Many people stay on SSRIs for years if their depression is recurrent. Long-term use is generally considered safe physically, but there are considerations: some side effects (like sexual dysfunction) can persist long-term, and there is debate about potential effects on brain chemistry after very prolonged use. Depression often returns if medication is stopped, so long-term therapy may be needed. Also, some long-term users report difficulty in discontinuing due to withdrawal symptoms. (On the flip side, decades of data show SSRIs can be life-changing and well-tolerated long-term for many individuals.) |
| Regulatory Status | Largely illegal; experimental – Psilocybin is classified as a Schedule I substance in the U.S., meaning it’s not legally available for medical use (outside of approved research trials). A few jurisdictions (like Oregon’s psilocybin therapy program and some decriminalized cities) have opened doors to legal use, but microdosing generally operates in a legal gray area. There are signs of change, with the FDA granting “Breakthrough Therapy” status to psilocybin for depression research and issuing guidance for clinical development. Still, at this time, microdosing is not an FDA-approved treatment. | Legal prescription medication – SSRIs are fully legal and regulated. They require a prescription in most countries, meaning a licensed healthcare provider must evaluate you and write an Rx. The medications are manufactured under strict quality control and approved by regulatory agencies (FDA, EMA, etc.) for treating depression, anxiety, and other conditions. Accessibility is high for those with a prescription. |
| Accessibility | Limited / “Grey Market” – Because of legal restrictions, obtaining psilocybin for microdosing can be challenging. Some people grow their own mushrooms or buy truffle microdose products in jurisdictions where that’s permitted. Others purchase from online dispensaries or local underground sources. Quality and dose consistency aren’t guaranteed unless you obtain products from a trusted source. (Note: Sugar Magnolia’s microdosing products – capsules, gummies, etc. – are an example of lab-tested, standardized options for those in areas where such products can be obtained legally or semi-legally.) | Widely available via healthcare – SSRIs can be obtained at any pharmacy with a doctor’s prescription. If you have health insurance, these medications are often covered or inexpensive as generics. Access to SSRIs depends on consulting with a doctor or psychiatrist who can evaluate if an antidepressant is appropriate. In terms of convenience, a daily pill from the pharmacy is straightforward to use, assuming one has medical oversight and can tolerate the medication. |
Interpreting the comparison: Psilocybin microdosing stands out for its rapid action, gentle side effect profile, and natural origins, but it is unregulated and still scientifically young. SSRIs are proven in large studies, easily accessible through doctors, and considered a standard of care, but they act slowly and can bring more pronounced side effects or withdrawal issues. Importantly, effectiveness varies individually – some people respond wonderfully to SSRIs, others do not; similarly, some may find microdosing life-changing, while others notice little effect. Personal brain chemistry and the nature of one’s depression/anxiety play a big role in determining which approach works best.
Next, we’ll look at what current research says about psilocybin’s antidepressant capabilities, and then discuss safety – especially regarding the combination of psilocybin and SSRIs.
What Does the Research Say About Psilocybin for Depression?
Clinical research on psilocybin (mostly using full psychedelic doses in therapeutic settings) has shown promising results for depression, including cases of major depressive disorder and treatment-resistant depression. In controlled trials, patients who received one or two guided psilocybin sessions often experienced significant reductions in depression scores within days, and improvements have lasted months for many participants. For example, a 2021 randomized trial compared psilocybin therapy (two high doses several weeks apart) with a daily SSRI (escitalopram) over six weeks. Both groups improved about the same on a standard depression scale – the psilocybin was not inferior to the SSRI – and notably about 57% of patients in the psilocybin group went into remission (no clinical depression), versus 28% in the SSRI group. Though the sample was relatively small, this hinted that psilocybin (with therapy) might achieve equal or greater outcomes in a fraction of the time that an SSRI takes. Other research at Johns Hopkins and elsewhere has found that a single high dose of psilocybin, paired with psychotherapy, can lead to rapid antidepressant effects that last 6 months to a year for some individuals. These findings have spurred Phase II and III trials in the U.S. and Europe, inching psilocybin closer to potential medical approval in the coming years.
When it comes to microdosing specifically, the research is still catching up to the hype. As discussed, much of the evidence so far comes from observational studies and self-reported surveys. These suggest a real signal that microdosing might improve mood and cognitive function in some people. Large-scale surveys (including one with over 8,700 respondents worldwide) found that microdosers reported lower levels of depression, anxiety, and stress compared to non-microdosing peers with similar backgrounds. Additionally, an open-label study by Fadiman and Korb (2019) collected reports from hundreds of microdosers and noted sustained mood improvements (especially for depression) over the 1.5-year study period.
On the other hand, placebo-controlled trials on microdosing have had mixed results. Some smaller studies found slight improvements in mood and creativity with microdoses of LSD or psilocybin, while others found that people felt better only if they believed they were microdosing (regardless of whether they actually got a placebo or not. This indicates expectation and the placebo effect can play a large role – which is not entirely surprising, as mindset is known to influence psychedelic experiences strongly. Researchers from University of Chicago (2022) conducted a lab-controlled psilocybin microdosing study and did not see the marked benefits that surveys reported, adding a note of caution.
In summary, high-dose psilocybin therapy has robust evidence supporting its antidepressant potential (enough that regulatory agencies are fast-tracking it), whereas microdosing’s efficacy remains an open question scientifically. It may work for some individuals, but more rigorous data is needed to determine for whom and under what conditions it helps. Importantly, virtually all experts agree that microdosing is not a guaranteed replacement for standard treatment – but it could be an alternative or complementary approach for those who cannot tolerate antidepressants or who seek a different path.
If you are considering psilocybin (in any dose) to address depression, it’s wise to do so under medical supervision, ideally in a therapeutic context. Depression is a serious condition; unproven remedies should not be used as a substitute for proven treatments without careful thought. That said, the paradigm of care may be expanding soon – a future where a trained professional might guide a patient in using psilocybin for depression (even microdosing) alongside talk therapy and lifestyle changes could become reality, pending ongoing research results.
Safety Considerations: Shrooms and SSRIs Together?
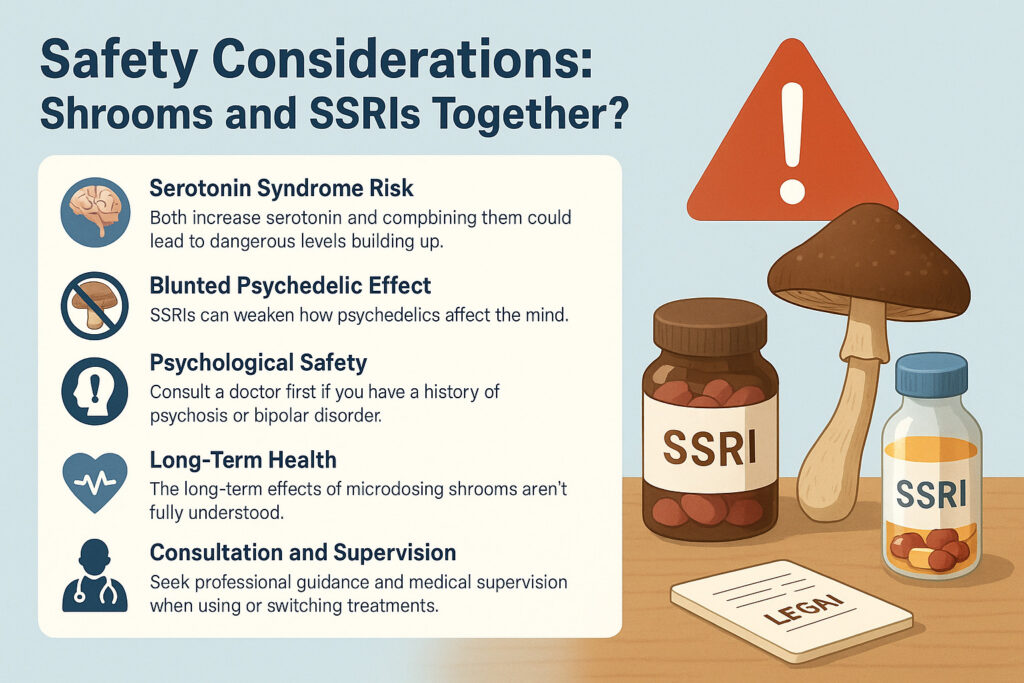
Whenever discussing psychedelics and antidepressants, a crucial topic is safety – particularly, what happens if someone mixes psilocybin with SSRI medications, or switches from one to the other. Here are key safety considerations to keep in mind:
- Serotonin Syndrome Risk: Both psilocybin and SSRIs increase serotonin activity in the brain, albeit in different ways. This raises the theoretical risk of serotonin syndrome, a dangerous condition caused by too much serotonin accumulating. In practice, serotonin syndrome from psychedelics is uncommon, but it can occur, especially if multiple serotonergic substances are combined. There is at least one documented case of a woman who was on a high-dose SSRI (venlafaxine, an SNRI) and started frequent psilocybin use; when her doctor added another serotonin-affecting drug (trazodone) to her regimen, she developed acute serotonin toxicity and had to be hospitalized. The combination of two antidepressants plus psilocybin likely pushed her serotonin levels over the edge. This case study highlights the danger of serotonin toxicity when psilocybin is used alongside antidepressants. The bottom line: if you are on an SSRI or similar antidepressant, do not add psilocybin (even as a microdose) without medical guidance. A doctor may advise tapering off the SSRI before initiating psilocybin therapy to reduce interaction risks. Serotonin syndrome can be life-threatening (symptoms include high fever, agitation, tremors, sweating, and rapid heart rate), so this is not a risk to take lightly.
- Blunted Psychedelic Effect: Interestingly, psychiatrists have noted that SSRIs might reduce the subjective effects of psychedelics. Many patients on SSRIs report that if they attempt a psychedelic experience, it feels weaker or produces less insight than expected. Early research supports this: SSRIs could attenuate psilocybin’s effects, possibly because the SSRI has already down-regulated certain serotonin receptors in the brain. What this means for microdosing is that if you are actively taking an SSRI, a microdose might feel like “nothing is happening” – or conversely, if you stop an SSRI to try microdosing, you might find psychedelics have a stronger effect once the SSRI is out of your system. Again, these scenarios should be navigated with a doctor’s help. You don’t want to yo-yo your brain chemistry on your own.
- Psychological Safety: Neither SSRIs nor microdoses typically cause dramatic psychological disturbances. However, anyone with a history of psychosis or certain bipolar types should be cautious. High-dose psychedelics can potentially trigger psychotic episodes in susceptible individuals; microdoses are less likely to do so, but robust data is lacking. SSRIs, on the other hand, carry an FDA warning about increased suicidal ideation in young people during initial use, and they can sometimes worsen anxiety before improving it. Monitoring by a healthcare provider is important when starting either treatment.
- Long-Term Health: As mentioned, microdosing’s long-term health impact is not fully known. One specific concern being researched is whether frequent psychedelic microdoses could affect the heart (through the 5-HT2B receptor, which, when agonized chronically, has been linked to heart valve issues in other contexts). So far there is no indication of this problem in microdosers, but it underlines why ongoing research and caution are warranted for chronic use of any substance. With SSRIs, long-term use is common and generally safe, but new findings (like post-SSRI sexual dysfunction persisting after cessation in some patients) show that we’re still learning about extended impacts of altering serotonin over years.
- Consultation and Supervision: Both SSRIs and psilocybin should ideally be taken with some form of professional guidance. For SSRIs, this means regular check-ins with a doctor to assess efficacy and side effects. For psilocybin (especially if macrodosing), it ideally means working with a therapist or facilitator experienced in psychedelic therapy. If you are self-medicating with microdoses, at the very least inform a healthcare provider of what you’re doing. They can help monitor your progress, and ensure there are no contraindications with other medications or conditions. Medical supervision is also critical if transitioning between SSRIs and psilocybin – typically a washout period is recommended (gradually taper off the SSRI, stay off for a couple weeks to clear it from your system, and only then consider psilocybin). This reduces the risk of interactions and allows each approach to work unimpeded.
- Legal Safety: As noted, using psilocybin outside of approved contexts carries legal risk. Possession of mushrooms or mushroom-based products could potentially lead to legal consequences in many jurisdictions. Always be aware of your local laws. Some people travel to retreat centers or jurisdictions where psilocybin use is permitted for a legal, guided experience instead of doing it clandestinely at home.
In summary, safety first. Psilocybin and SSRIs both affect the serotonin system, and mixing them is not something to do casually. If you’re currently on antidepressants and are curious about microdosing, talk to your doctor about it. They can help devise a plan, which might involve sticking with your current treatment (if it’s working), or safely transitioning to a different approach. And if you ever experience symptoms like those of serotonin syndrome or any alarming reaction, seek medical help immediately.
Approachable Microdosing Options (Product Promotion)
If you’ve consulted with your healthcare provider and decided to explore microdosing as a wellness practice, one challenge you might face is finding a reliable, consistent product. Dosing accuracy is crucial – too little might do nothing, too much might take you beyond a microdose. That’s where Sugar Magnolia’s curated microdosing products can help. They offer an approachable way for adults to try microdosing with built-in consistency and quality. Here are some options:
- Microdose Capsules – Sugar Magnolia’s capsules contain pre-measured microdoses of psilocybin in an easy-to-swallow pill form. Capsules are ideal if you want precise dosing (no guesswork) and a flavorless, convenient format. You can seamlessly fit them into your daily vitamin or supplement routine. Each capsule provides a controlled amount of our premium mushroom blend, so you know exactly how much you’re taking.
- Psilocybin Chocolate Bar – For those who prefer to pair wellness with a treat, our chocolate bar is a delicious option. This artisanal bar infuses a carefully calibrated microdose of psilocybin into each square of chocolate. Not only do you get the mood-enhancing benefits of mushrooms, but you also get to savor gourmet-quality chocolate – making your microdosing ritual both enjoyable and discreet. It’s a fantastic choice if you don’t like the taste of mushrooms or want a more indulgent experience.
- Gummies (200 mg) – Sugar Magnolia’s standard microdose gummies provide 200 mg of our special mushroom blend per gummy (which is within the typical microdose range). These fruity gummies are vegan, made with organic ingredients, and taste just like a little candy treat. Gummies are perfect for those who want a chewable, shareable form of microdosing. They’re easy to split or adjust if you want to start with an even smaller dose, and they come in a resealable package to keep them fresh. Many people find gummies to be an approachable entry point into microdosing because the format is friendly and familiar.
- High-Potency Gummies (500 mg) – For experienced microdosers or those who find they need a slightly stronger dose, Sugar Magnolia offers a 500 mg gummy option. Each gummy in this pack contains 0.5 grams of our Albino Penis Envy/Avery mushroom blend – still a sub-psychedelic dose, but on the higher end of the microdose spectrum. These are great for individuals who have built some tolerance or whose body chemistry benefits from a bit more psilocybin. Despite the higher dose, they’re crafted with the same care: natural flavors, organic cane sugar, and consistent potency in every piece. We always recommend starting lower (with 200 mg) and only moving up to 500 mg if needed, as everyone’s sensitivity differs.
All Sugar Magnolia products undergo rigorous quality control (our PsiloSafe certification process) to ensure purity, accurate dosing, and safety. The mushrooms are expertly curated and blended, so you’re getting a consistent experience each time. These products remove a lot of the uncertainty from microdosing – you won’t have to worry about potency variations or measuring powders yourself. Plus, they are discreet and travel-friendly, resembling everyday wellness products.
Important: Even though these products make microdosing easier, they are intended for use by responsible adults in appropriate settings. Please keep them out of reach of children and pets. And as always, if you have an underlying health condition or are taking other medications (especially SSRIs or other psychiatric meds), consult your healthcare provider before using psilocybin products.
Conclusion and Next Steps
Both shrooms and SSRIs offer paths to improving mood, but they come from very different worlds – one is a natural psychedelic with ancient roots and cutting-edge research behind it, the other is a modern pharmaceutical with decades of widespread use. In weighing this mood booster comparison, it’s not about declaring an absolute winner, but about finding what’s most suitable for you. Some may find that SSRIs provide steady relief and are the right choice for their mental health journey. Others may be intrigued by the idea of psilocybin microdosing as a more holistic or innovative approach, either as an alternative or a complement to traditional therapy. In certain cases, a person might even benefit from both (at different times or under professional guidance).
The key takeaways are: do your research, consult professionals, and listen to your body. If an SSRI isn’t working or its side effects are too burdensome, it’s understandable to seek a new solution like microdosing – just do so safely. On the flip side, if you’re microdosing and not achieving the desired results, you might need the heavier artillery of a conventional antidepressant or therapy. There is no one-size-fits-all in mental health. Depression and anxiety are complex, and what works for one person may not work for another.
For those curious to give microdosing a try, My Sugar Magnolia provides an accessible entry point. You can explore our range of microdosing products mentioned above – each designed to take the guesswork out of the process. Starting with a low, controlled dose in a supportive environment can make all the difference in having a positive experience. And remember, psilocybin is not a magic bullet; think of it as a tool that works best alongside healthy lifestyle choices, therapy, mindfulness, and support from others.
Speaking of support, we warmly invite you to become part of our community. If you’re passionate about plant medicine and want to connect with others on this journey, consider joining our Sugar Mama program. As a Sugar Mama ambassador, you’ll be part of a welcoming community and enjoy exclusive perks – from wholesale pricing on products to sharing experiences and tips with like-minded individuals. It’s a chance to deepen your engagement and help cultivate a culture of responsible, educated plant medicine use.
Ready to take the next step?
Whether you decide to stick with SSRIs, try microdosing, or carefully combine approaches, the goal is better mental well-being. Always prioritize safety and professional guidance in your choices. If you’re ready to explore the natural route, check out My Sugar Magnolia’s product line and resources. And if you feel inspired to share the journey, join the Sugar Mama movement for support and community. Your mental health is worth nurturing with the best of both modern science and natural wisdom. Here’s to finding the balance that works for you, and to brighter days ahead.

